What is causing pain at the front of my knee?
5 CommentsMany athletes and recreational sports people suffer from on-going knee pain and soreness. Today Physiotherapist Sarah Marshall looks in more detail at one aspect.
One of the most common types is Anterior Knee Pain (AKP). It describes pain at the front of the knee and can affect up to 40% of the population. It is especially common amongst athletes, yet not disrupt their sporting function or ability.
What are the causes of AKP?
There are many causes of AKP and I have listed the most common below. Symptoms will often present without specific injury. Any persistent pain must be assessed by an appropriate medical professional in order to make an accurate diagnosis who will then advise on the correct treatment plan.
Patello-Femoral Joint Pain (PFJP) is by far the most common cause of AKP. Athletes will describe pain in and around the patella. I would not expect to see any significant swelling around the knee joint.
Symptoms are usually aggravated by stairs, kneeling, squatting, lunging and running. PFJP can also cause pain at rest, especially when sitting for long periods (movie goer’s knee).
A Patella Tendonopathy, Fat Pad Irritation / Impingement, Bursitis and Patella Instability with also produce AKP.
What causes PFJP
There are many contributing factors to the development of PFJP
- Local muscle weakness (especially quadriceps)
- Poor neuromuscular control
- Muscle tightness (especially quadriceps and hamstrings)
- Poor hip / pelvic control / stability
- Poor foot posture / mechanics
All of the above will increase the functional loading of the Patello-Femoral Joint which is likely to cause inflammation and pain with repeated use. PFJP is also a very common complaint following any knee joint surgery and must not be missed as referred pain from an old Posterior Cruciate Ligament injury.
Management of PFJP

Get your knee assessed by a Chartered Physiotherapist
Always seek professional advice if you can before embarking on a rehabilitation programme. Initially, pain levels need to be managed and controlled before early rehabilitation can be progressed.
Pain Management
- Activity modification i.e. avoid aggravating factors
- Taping techniques
- Acupuncture
- Soft tissue massage
Rehabilitation
- Stretching programme (hamstrings, quadriceps, gastrocnemius, anterior hip structures)
- A graded strengthening programme with initial emphasis on quadriceps
- Hip and pelvis stability exercises ( transversus abdominus, gluteus medius)
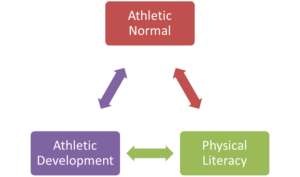
(Post rehab, there are 3 keys to maintaining Knee Health)
There are limited surgical options for this problem with relatively poor outcomes.
A biomechanical assessment of the foot can help determine whether shoes orthotics are indicated. Commitment to rehabilitation must be adhered to for many months in order to achieve individual goals.
Unfortunately, without the appropriate management, PFJP often develops into a chronic problem.
If you want an individual assessment on your knee pain, then please book in to see me.
Sarah Marshall










 Planning: The best place to start is to look at the next 4 weeks. Use this free
Planning: The best place to start is to look at the next 4 weeks. Use this free  Strength/co-ordination training: It is the ability to control your own body throughout the match and the season that is the key to avoid getting injured. Your exercise programme has to be specific for young athletes: time spent on crosstrainers, exercise bikes and lying down on a bench is time wasted.
Strength/co-ordination training: It is the ability to control your own body throughout the match and the season that is the key to avoid getting injured. Your exercise programme has to be specific for young athletes: time spent on crosstrainers, exercise bikes and lying down on a bench is time wasted.


 Bill Knowles doesn’t have any magic answers or quick fix exercises. His approach to injury rehabilitation based on good coaching and insisting on excellence in every exercise means injured athletes getting back to competition readiness sooner.
Bill Knowles doesn’t have any magic answers or quick fix exercises. His approach to injury rehabilitation based on good coaching and insisting on excellence in every exercise means injured athletes getting back to competition readiness sooner. LCA
LCA The previous recommendations by the ACPSM were made based on evidence published up to 1996. These current clinical guidelines, which I have summarised below, were produced by a team of volunteers using evidence up to 2010. Each PRICE intervention has been graded as STRONG, WEAK or UNCERTAIN.
The previous recommendations by the ACPSM were made based on evidence published up to 1996. These current clinical guidelines, which I have summarised below, were produced by a team of volunteers using evidence up to 2010. Each PRICE intervention has been graded as STRONG, WEAK or UNCERTAIN. “Probably use compression/elevation after an acute soft tissue injury”. WHY?
“Probably use compression/elevation after an acute soft tissue injury”. WHY?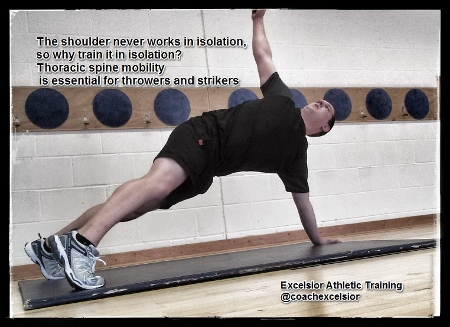 Start to work on low level movement and control exercises. This includes extended press ups either against the wall or on the floor, shoulder rolls, shrugs, and protraction exercises.
Start to work on low level movement and control exercises. This includes extended press ups either against the wall or on the floor, shoulder rolls, shrugs, and protraction exercises. Children and adolescents endure many of the same injuries and mechanical dysfunctions as adults. However, in the maturing skeleton there are some specific conditions that are only seen in the young.
Children and adolescents endure many of the same injuries and mechanical dysfunctions as adults. However, in the maturing skeleton there are some specific conditions that are only seen in the young. Monitor and keep a record of the child’s growth. This can help to adapt training needs specifically .e.g. during a growth spurt an increased emphasis on stretching is required and maybe some reduced activity.
Monitor and keep a record of the child’s growth. This can help to adapt training needs specifically .e.g. during a growth spurt an increased emphasis on stretching is required and maybe some reduced activity.